Spotlight on R&D - Tina Baharlou, Industrial Placement Student
.png?la=en-gb&h=250&w=250&hash=B341FC472F18012F6BDC461540845881) Can you share a bit about your background and what led you to do a placement?
Can you share a bit about your background and what led you to do a placement?
I’m currently studying for an integrated master’s in chemistry with Medicinal Chemistry at Newcastle University. I chose to do a year in industry to gain practical experience and see how research is applied in real-world settings. Alongside my placement, I continued my university studies, which helped me connect academic learning with day-to-day lab work.
I’ve really enjoyed seeing how my work contributes to solving real formulation challenges, particularly through my project focused on the delivery of biologics via soft mist inhalers and nebulisers. Attending conferences has given me a broader understanding of the industry, and collaborating with marketing teams has shown how research supports product development and customer needs. Overall, the placement has boosted my confidence, improved my lab and communication skills, and given me a clearer idea of the career path I want to follow.
What are the biggest challenges you’ve encountered with protein or biologic formulations?
One of the key challenges in biologic formulation is maintaining protein integrity under stress, whether from mechanical forces, nebulisation, or chemical degradation. Biologics are inherently sensitive molecules, and their structure can be easily disrupted by physical and chemical stressors. In my work, I’ve focused on surfactants such as polysorbates (Tween™) and sorbitan esters (Span™), studying how excipient purity and processing conditions impact long-term stability. Even minor impurities or the absence of stabilisers like Ethylenediaminetetraacetic acid (EDTA) or α-tocopherol can significantly influence aggregation behaviour and particle size distribution.
Delivering biologics via inhalation adds another layer of complexity. Nebulisers expose proteins to additional mechanical stresses, and formulation compatibility with the device is critical. Moreover, a major regulatory challenge is the limited number of FDA approved excipients for pulmonary delivery. Many commonly used stabilisers in parenteral formulations aren't yet accepted for inhalation, which narrows formulation options and makes achieving both stability and safety more difficult. This means every component must be carefully selected to balance efficacy, safety, and performance, making biologic delivery via inhalation one of the more technically demanding areas of formulation science.
One area I find particularly exciting is the advancement of soft mist inhalers (SMIs) as a platform for delivering biologics. Traditionally used for small molecule drugs, SMIs are now being explored for more complex therapeutics like proteins, peptides, and even lipid nanoparticles (LNPs). They offer several advantages such as low shear stress, no need for propellants, and consistent aerosol performance, which make them a promising option for pulmonary delivery of sensitive molecules.
Working with these devices has allowed me to directly observe the differences in formulation behaviour before and after nebulisation. Using analytical techniques like dynamic light scattering (DLS)to assess particle size and stability has highlighted how both the formulation and the delivery device influence overall performance.
As these technologies advance, integrating analytical techniques into a cohesive workflow is becoming increasingly important. It enables a more informed, data driven approach to formulation development. With growing interest in inhaled biologics, and a push to expand the excipient options available for pulmonary use, it’s a particularly exciting time to be involved in this area of research.
One of the most important lessons I’ve learned is that excipient selection is not just about compatibility. It is also about ensuring performance, maintaining stability, and supporting scalability. I’ve seen how excipients such as polysorbates can behave very differently depending on their purity, and how optimising even minor components of a formulation can significantly improve its robustness. I’ve also learned the importance of data consistency and reproducibility, especially when working with biologics, where even small variations can potentially impact product quality.
Outside of the lab, I enjoy playing hockey, swimming, and going to the gym. I’m also a big traveller, I love exploring new places, especially natural landscapes like mountains, lakes, and coastlines. Experiencing different cultures and trying local foods is one of my favourite parts of travelling. It always gives me a fresh perspective and a chance to recharge.
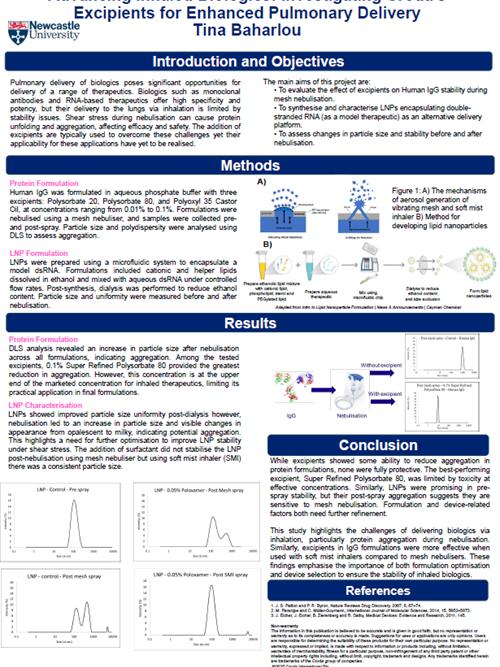
My poster focuses on the challenges of delivering biologics via inhalation and explores how Croda’s excipients can help improve stability during nebulisation. I investigated Human IgG formulations with different Super Refined™ surfactants and evaluated their ability to reduce protein aggregation during mesh nebulisation. I also formulated LNPs encapsulating model double-stranded RNA using a microfluidic system and assessed their stability before and after nebulisation.
One of the key findings was that while some excipients, such as Super Refined™ Polysorbate 80, reduced aggregation, the effective concentrations approached the upper limits currently used for inhaled formulations. Similarly, LNPs were promising in terms of pre-spray stability, but tended to aggregate post-nebulisation, especially when delivered via mesh nebulisers. However, the delivery of double-stranded RNA using a SMI with Super Refined™ Poloxamer 188 was successful in preventing aggregation and maintaining consistent particle size, demonstrating a more viable route for inhaled RNA-based therapeutics. These findings highlight the critical importance of both formulation strategy and device selection in the development of stable and effective inhaled biologics.
If you're interested, you can download a copy of the poster here
Advancing inhaled biologics: Investigating Croda’s excipients for enhanced pulmonary delivery